In health care settings, personal protective equipment (PPE) refers to specialized clothing or equipment used to prevent the spread of infection, including gloves, gowns, facial protection (masks and eye protection), and respirators. PPE is a barrier that protects the health care worker from exposure to infectious agents and also prevents the transmission of microorganisms to other individuals including staff, patients, and visitors.
Gloves
Gloves are disposable, one-time-use coverings that protect the hands of health care providers. See Figure 4.7[1] for an image of nonsterile medical gloves in various sizes in a health care setting. Gloves are used to protect the hands of a health care worker from coming into contact with a client’s potentially infected body fluids and to protect patients from coming into contact with potential contaminants on health care workers’ hands during certain procedures and treatments. Gloves should also be worn by a health care worker when there is a risk of transmitting their own body fluids from nonintact skin on their hands to other individuals. However, gloves should not be worn for routine activities such as taking vital signs or transferring a client in a wheelchair unless indicated due to transmission-based precautions.

Gloves are typically made from latex, nitrile, and vinyl. Many people are allergic to latex, so be sure to check for latex allergies for the patient and other members of the health care team. Most gloves are not hand-specific and can be worn on either the left or right hand. Gloves come in a variety of sizes such as small, medium, large, and extra large and should have a snug fit, not too tight or too loose, to provide better protection to the health care provider.[2]
Gloves should always be used in combination with proper hand hygiene that is performed prior to applying gloves and repeated again after gloves are removed. Gloves are task-specific and should not be worn for more than one task or procedure on the same client because some tasks may have a greater concentration of microorganisms than others. For example, gloves are worn to assist a client with incontinent care, but gloves should be removed, hand hygiene performed, and new gloves applied before assisting with oral care. Gloves should never be reused or washed to be reused. Reusing gloves has been linked with the transmission of infectious microorganisms.
Gloves should never replace hand hygiene for several reasons[3]:
- Gloves may have imperfections such as holes or cracks that are not visible.
- Hands may have become contaminated while removing the gloves.
- Gloves may have become damaged while wearing.
Fingernails should be short prior to applying gloves so they do not puncture the gloves. Put on (don) gloves after hands are completely dry after performing hand hygiene. There is no specific method for putting on gloves, but care should be taken when donning gloves to avoid tearing. Gloves should be applied so they completely cover the wrists. Gloves must be removed carefully, followed by proper hand hygiene, to prevent the spread of infection.[4]
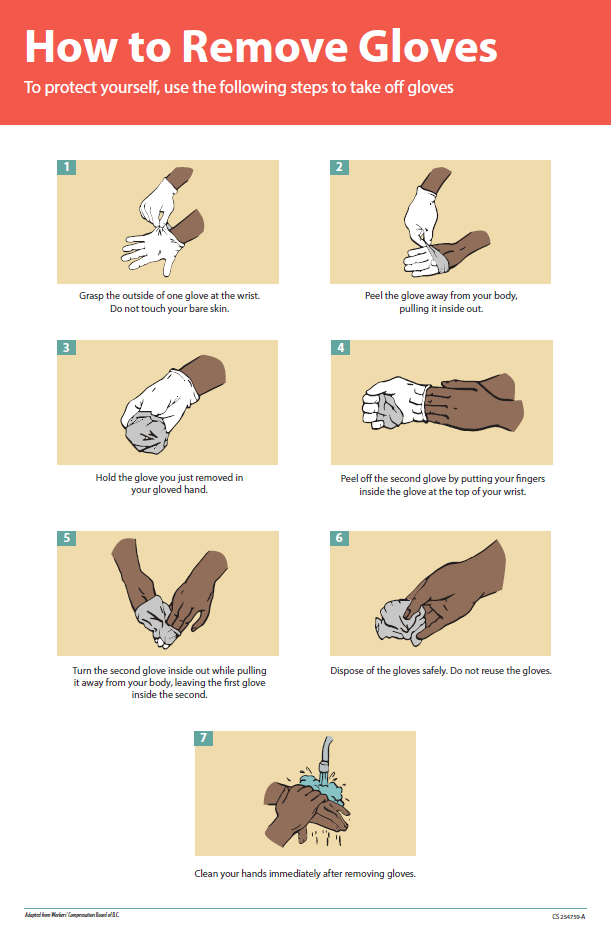
Removing Gloves
See Figure 4.8[5] for an illustration of properly removing gloves. Hand hygiene should be performed following glove removal to ensure the hands will not carry potentially infectious agents that might have penetrated through unrecognized tears or contaminated the hands during glove removal.
Properly removing gloves includes the following steps[6]:
- Grasp the outside of one glove near the wrist. Do not touch your skin.
- Peel the glove away from your body, pulling it inside out.
- Hold the removed glove in your gloved hand.
- Put your fingers inside the glove at the top of your wrist and peel off the second glove.
- Turn the second glove inside out while pulling it away from your body, leaving the first glove inside the second.
- Dispose of the gloves safely. Do not reuse.
- Perform hand hygiene immediately after removing the gloves.
Review infection prevention and control practices related to glove usage in the following interactive activity.
This work is a derivative of Infection Prevention and Control Practices by Michelle Hughes and Kendra Allen is licensed under CC BY 4.0.
Isolation Gowns
Isolation gowns are protective garments worn to protect clothing from the splashing or spraying of body fluids and reduce the transmission of microorganisms. Isolation gowns can be disposable or reusable. The gowns should have long sleeves with a snug fit at the wrist, cover both the front and the back of the body from the neck to the thighs, and overlap at the back.
Gloves should fit over the cuffs of the gown. Gowns should fasten at the neck and waist using ties, snaps, or Velcro.[7]
Disposable gowns are made from materials that make them resistant to fluids. Reusable gowns are made of tightly woven cotton or polyester and are chemically finished to improve their ability to be fluid resistant; they are laundered after each use. Gowns are considered task-specific and should be changed if they become heavily soiled or damaged. Isolation gowns should be put on immediately prior to providing client care and should be removed immediately after care is completed before leaving the room. After use, gowns should be discarded into an appropriate receptacle for disposal or to be laundered if the gown is reusable. See Figure 4.9[8] for an image of an isolation gown.

Special care should be taken when removing the gown to prevent contamination of clothing and skin. The front of the gown is always considered to be contaminated. Ties at the front are considered contaminated, but ties at the side and the back are considered uncontaminated.[9]
See the “Donning/Doffing PPE” checklists later in this chapter for steps for proper removal of gowns. Review information related to using isolation gowns in the following interactive activity.
This work is a derivative of Important Considerations When Wearing Gowns by Audrey Kenmir and is licensed under CC BY 4.0.
Eye Protection
Eye protection in health care settings includes face shields, visors attached to masks, and goggles that are used to protect the eyes from blood or body fluids. Eye protection should be worn by health care workers during patient care when there may be splashing or spraying of body fluids or within six feet of a coughing client. For example, eye protection is worn when emptying a urinary catheter or assisting a nurse in irrigating a wound or suctioning a client’s airway.
Eye protection can be disposable, like face shields, or reusable, like eye goggles. If eye protection is reusable, it should be cleaned before reuse. Face shields and visors attached to masks offer better visibility than goggles. Eye protection should fit comfortably and securely while allowing for visual acuity. Eyeglasses can be worn under face shields or goggles.[10] See Figure 4.10[11] for an image of eye goggles with and without a face shield.

Review information related to the use of eye protection in the following learning activity.
This work is a derivative of Important Considerations When Wearing Eye Protection by Michelle Hughes and is licensed under CC BY-NC 4.0.
Masks
Masks are protective coverings worn by health care providers to protect the mucous membranes of their nose and mouth. In long-term care settings, masks are typically secured by elastic loops around the ears. The top edge of the mask has a bendable strip to secure the seal of the mask over the bridge of the nose. Some situations require masks to be combined with a face shield or a visor that covers the eyes. See Figure 4.11[12] for an image of masks used with eyeglasses and an eyeshield.

Medical masks should be worn when providing care that may cause splashing or spraying of blood or body fluids or within six feet of a client who is coughing or has been placed in droplet precautions. Medical masks should also be worn by health care providers who are coughing to prevent transmission of exhaled respiratory droplets to clients.
Medical masks can differ in their filtration effectiveness and the way in which they fit. Single-use disposable medical masks are effective when providing care to most clients and should be changed when damp or soiled. When medical masks become moist, they may not provide an effective barrier to microorganisms. A medical mask, when properly worn, should fit snugly over the nose, mouth, and under the chin so that microorganisms and body fluids cannot enter or exit through the sides of the mask. If the health care worker wears glasses, the glasses should be placed over the top edge of the mask. This will help prevent the glasses from becoming foggy as the person wearing the mask exhales.
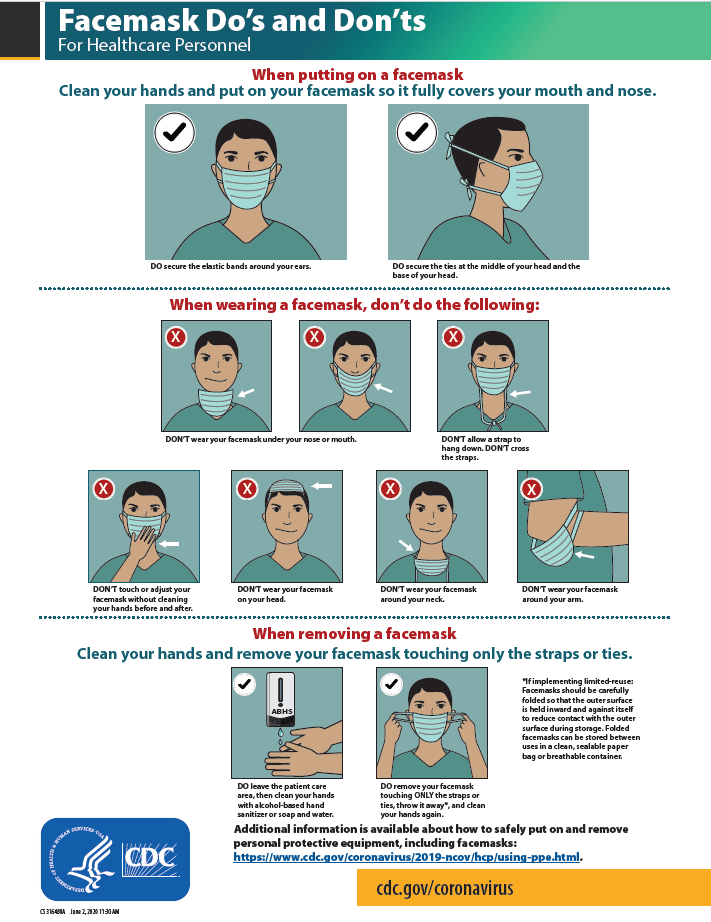
Removing Facemasks
Like the isolation gown, the front of the mask is considered contaminated. The mask should be removed by taking the ear loop off and placing it in the appropriate disposal area. It is important to properly remove masks to avoid contamination. See Figure 4.12[13] for an illustration of how to remove a facemask according to the CDC. See the “Donning/Doffing PPE With a Mask and Face Shield or Goggles” checklist for more details.
This work is a derivative of Important Considerations When Wearing Medical Masks by Michelle Hughes and is licensed under CC BY 4.0.
This work is a derivative of Important Considerations When Wearing Medical Masks by Michelle Hughes and is licensed under CC BY 4.0.
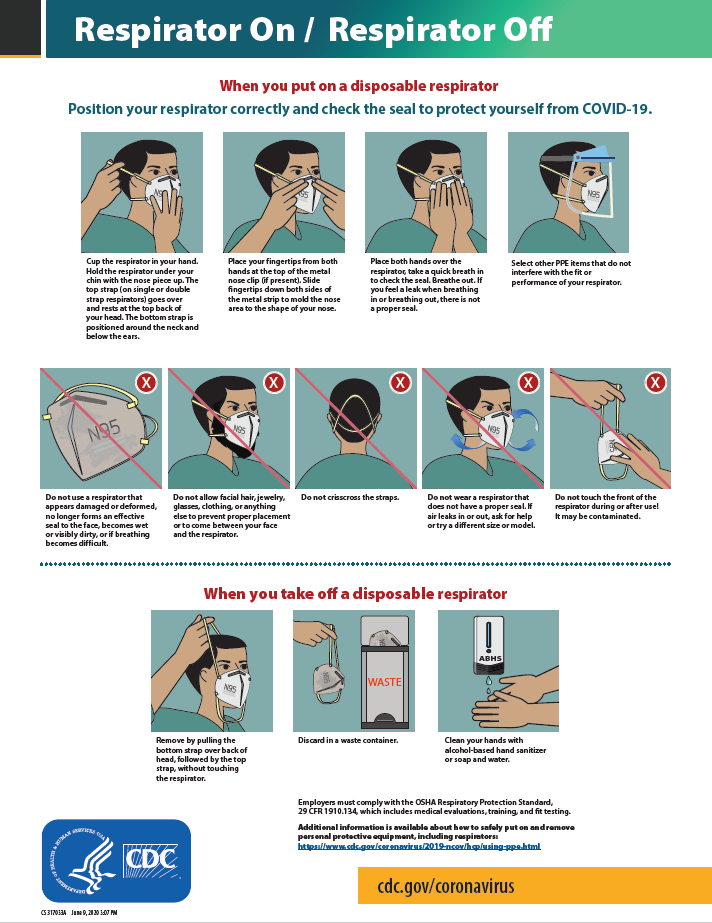
Respirators and PAPRs
Residents requiring airborne transmission precautions are transferred to a hospital immediately upon suspicion or confirmation of an airborne illness as respiratory protection used with airborne transmission precautions requires special equipment. Respirator masks with N95 or higher filtration are worn by health care professionals to prevent inhalation of infectious small airborne particles. It is important to apply, wear, and remove respirators appropriately to avoid contamination. A user-seal check should be performed by the wearer each time a respirator is donned to minimize air leakage around the facepiece. See Figure 4.13[14] for CDC recommendations when wearing disposable respirators.
A newer piece of equipment used for respiratory protection is the powered air-purifying respirator (PAPR). A PAPR is an air-purifying respirator that uses a blower to force air through filter cartridges or canisters into the breathing zone of the wearer. This process creates an air flow inside either a tight-fitting facepiece or loose-fitting hood or helmet, providing a higher level of protection against aerosolized pathogens, such as COVID-19, during respiratory suctioning. See Figure 4.14[15] for an example of PAPR in use.

Resident Considerations During Isolation Precautions
There are a lot of things to consider when preventing the spread of infection among residents, staff, equipment, and surfaces. It is important to think about the tasks you will be performing for residents and determine ahead of time what you might be exposed to in order to select the appropriate PPE. The perspective and needs of clients placed in isolation precautions should also be considered. PPE makes communication more difficult by hiding facial expressions and making hearing more difficult, and therapeutic touch is less personal when wearing gloves. Caregivers often spend less time interacting with clients in transmission-based precautions due to the labor intensiveness of putting on and taking off PPE, resulting in clients often developing feelings of loneliness and social isolation due to less frequent interactions. Try to keep the resident’s routine as normal as possible and apply extra effort to interact with the client.
When transporting a client with transmission-based precautions within a facility, keep these principles in mind[16]:
- Limit transport for essential purposes only, such as diagnostic and therapeutic procedures that cannot be performed in the patient’s room.
- When transporting, use appropriate barriers on the patient consistent with the route and risk of transmission. For example, for a resident with a skin infection with MRSA, be sure the area is covered.
- Notify health care personnel in the receiving area of the impending arrival of the patient and of the precautions necessary to prevent transmission.
- “Surgery Centre Accriditation.jpg” by Accredia is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Introduction to Infection Prevention and Control Practices for the Interprofessional Learner by Hughes, Kenmir, St-Amant, Cosgrove, & Sharpe and is licensed under CC BY-NC 4.0 ↵
- This work is a derivative of Introduction to Infection Prevention and Control Practices for the Interprofessional Learner by Hughes, Kenmir, St-Amant, Cosgrove, & Sharpe and is licensed under CC BY-NC 4.0 ↵
- This work is a derivative of Introduction to Infection Prevention and Control Practices for the Interprofessional Learner by Hughes, Kenmir, St-Amant, Cosgrove, & Sharpe and is licensed under CC BY-NC 4.0 ↵
- “poster-how-to-remove-gloves.pdf” by Centers for Disease Control and Prevention is in the Public Domain. Access for free at https://www.cdc.gov/vhf/ebola/resources/posters.html ↵
- Siegel, J. D., Rhinehart, E., Jackson, M., Chiarello, L., & Healthcare Infection Control Practices Advisory Committee. (2019, July 22). 2007 guideline for isolation precautions: Preventing transmission of infectious agents in healthcare settings. Centers for Disease Control and Prevention. https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html ↵
- This work is a derivative of Introduction to Infection Prevention and Control Practices for the Interprofessional Learner by Hughes, Kenmir, St-Amant, Cosgrove, & Sharpe and is licensed under CC BY-NC 4.0 ↵
- “U.S. Navy Doctors, Nurses and Corpsmen Treat COVID Patients in the ICU Aboard USNS Comfort (49825651378).jpg” by Navy Medicine is in the Public Domain ↵
- This work is a derivative of Introduction to Infection Prevention and Control Practices for the Interprofessional Learner by Hughes, Kenmir, St-Amant, Cosgrove, & Sharpe and is licensed under CC BY-NC 4.0 ↵
- This work is a derivative of Introduction to Infection Prevention and Control Practices for the Interprofessional Learner by Hughes, Kenmir, St-Amant, Cosgrove, & Sharpe and is licensed under CC BY-NC 4.0 ↵
- “IMG_2021-scaled” and “IMG_2026-scaled” by unknown author are licensed under CC BY-NC-4.0. Access for free at https://ecampusontario.pressbooks.pub/introductiontoipcp/chapter/eye-protection/ ↵
- “Screen-Shot-2021-05-05-at-3.57.19-PM” and “Screen-Shot-2021-05-05-at-3.57.41-PM” by unknown author are licensed under CC BY-NC 4.0. Access for free at https://ecampusontario.pressbooks.pub/introductiontoipcp/chapter/masks/ ↵
- “fs-facemask-dos-donts.pdf” by Centers for Disease Control and Prevention is in the Public Domain. Access for free at https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html ↵
- “fs-respirator-on-off.pdf” by Centers for Disease Control and Prevention is in the Public Domain. Access for free at https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html ↵
- “PAPRs_in_use_01.jpg" by Ca.garcia.s is licensed under CC BY-SA 4.0 ↵
- Siegel, J. D., Rhinehart, E., Jackson, M., Chiarello, L., & Healthcare Infection Control Practices Advisory Committee. (2019, July 22). 2007 guideline for isolation precautions: Preventing transmission of infectious agents in healthcare settings. Centers for Disease Control and Prevention. https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html ↵
Equipment used to prevent transmission of blood-borne pathogens and infection, including gloves, masks, goggles, gowns, and other types of protective equipment.
Protective coverings worn by health care providers to protect the mucous membranes of their nose and mouth. In long-term care settings, masks are typically secured by elastic loops around the ears.
An air-purifying respirator that uses a blower to force air through filter cartridges or canisters into the breathing zone of the wearer.
