The chain of infection, also referred to as the chain of transmission, describes how an infection spreads based on these six links of transmission:
- Infectious Agent
- Reservoirs
- Portal of Exit
- Modes of Transmission
- Portal of Entry
- Susceptible Host
See Figure 4.1[1] for an illustration of the chain of infection. If any “link” in the chain of infection is removed or neutralized, transmission of infection will not occur. Health care workers must understand how an infectious agent spreads via the chain of transmission so they can break the chain and prevent the transmission of infectious disease. Routine hygienic practices, standard precautions, and transmission-based precautions are used to break the chain of transmission.
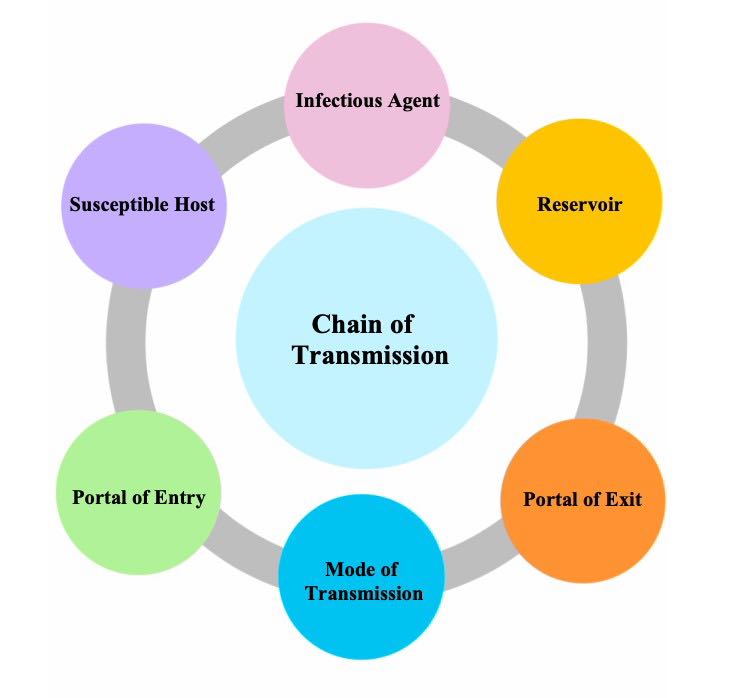
The links in the chain of infection include Infectious Agent, Reservoir, Portal of Exit, Mode of Transmission, Portal of Entry, and Susceptible Host[2]:
- Infectious Agent: Microorganisms, such as bacteria, viruses, fungi, or parasites, that can cause infectious disease.
- Reservoir: The host in which infectious agents live, grow, and multiply. Humans, animals, and the environment can be reservoirs. Examples of reservoirs are a person with a common cold, a dog with rabies, or standing water with bacteria. Sometimes a person may carry an infectious agent but is not symptomatic or ill. This is referred to as being colonized, and the person is referred to as a carrier. For example, many health care workers carry methicillin-resistant Staphylococcus aureus (MRSA) bacteria in their noses but are not symptomatic.
- Portal of Exit: The route by which an infectious agent escapes or leaves the reservoir. In humans, the portal of exit is typically a mucous membrane or other opening in the skin. For example, pathogens that cause respiratory diseases usually escape through a person’s nose or mouth.
- Mode of Transmission: The way in which an infectious agent travels to other people and places because they cannot travel on their own. Modes of transmission include contact, droplet, or airborne transmission. For example, touching sheets with drainage from one person’s infected wound and then touching another person without washing one’s hands is an example of contact transmission of an infectious agent. Examples of droplet or airborne transmission are coughing and sneezing, depending on the size of the microorganism.
- Portal of Entry: The route by which an infectious agent enters a new host (i.e., the reverse of the portal of exit). For example, mucous membranes, skin breakdown, and artificial openings in the skin created for the insertion of medical equipment (such as intravenous lines) are at high risk for infection because they provide an open path for microorganisms to enter the body. Tubes inserted into mucous membranes, such as a urinary catheter, also facilitate the entrance of microorganisms into the body. A person’s immune system fights against infectious organisms that have entered the body through the use of nonspecific and specific defenses. Read more about defenses against microorganisms in the “Defenses Against Transmission of Infection” section of this chapter.
- Susceptible Host: A person at elevated risk for developing an infection when exposed to an infectious agent due to changes in their immune system defenses. For example, infants (up to 2 years old) and older adults (aged 65 or older) are at higher risk for developing infections due to underdeveloped or weakened immune systems. Additionally, anyone with chronic medical conditions (such as diabetes) are also at higher risk of developing an infection. In health care settings, almost every patient is considered a “susceptible host” because of preexisting illnesses, medical treatments, medical devices, or medications that increase their vulnerability to developing an infection when exposed to infectious agents in the health care environment. As caregivers, it is the NA’s responsibility to protect susceptible patients by breaking the chain of infection.
After a susceptible host becomes infected, they become a reservoir that can then transmit the infectious agent to another person. If an individual’s immune system successfully fights off the infectious agent, they may not develop an infection, but instead the person may become an asymptomatic “carrier” who can spread the infectious agent to another susceptible host. For example, individuals exposed to COVID-19 may not develop an active respiratory infection but can spread the virus to other susceptible hosts via sneezing.
Learn more about the chain of infection by clicking on the following activities.
This H5P activity is a derivative of original activities by Michelle Hugues and licensed under CC BY-NC 4.0 unless otherwise noted.
This H5P activity is a derivative of original activities by Michelle Hugues and licensed under CC BY-NC 4.0 unless otherwise noted.
This H5P activity is a derivative of original activities by Michelle Hugues and licensed under CC BY-NC 4.0 unless otherwise noted.
This H5P activity is a derivative of original activities by Michelle Hugues and licensed under CC BY-NC 4.0 unless otherwise noted.
This H5P activity is a derivative of original activities by Michelle Hugues and licensed under CC BY-NC 4.0 unless otherwise noted.
This H5P activity is a derivative of original activities by Michelle Hugues and licensed under CC BY-NC 4.0 unless otherwise noted.
Putting It All Together
Note: To enlarge the print, you can expand the activity by clicking the arrows in the right upper corner of the text box. Please drag and drop the descriptors and actions into the appropriate boxes to demonstrate the various steps in the chain of infection.
This H5P activity is a derivative of original activities by Michelle Hugues and licensed under CC BY-NC 4.0 unless otherwise noted.
Healthcare-Acquired Infections
An infection that develops in an individual after being admitted to a health care facility or undergoing a medical procedure is a healthcare-associated infection (HAI), formerly referred to as a nosocomial infection. About 1 in 31 hospital patients develops at least one healthcare-associated infection every day. HAIs increase the cost of care and delay recovery. They are associated with permanent disability, loss of wages, and even death. An example of an HAI is a skin infection that develops in a patient’s incision after they had surgery due to improper hand hygiene of health care workers.[3],[4] It is important to understand the dangers of Healthcare-Acquired Infections and actions that can be taken to prevent them.
Read more details about healthcare-acquired infections in the “Infection” chapter of Open RN Nursing Fundamentals.
Healthcare-Associated Infections by Michelle Hughes is licensed under CC BY 4.0.
- “Chain-of-Transmission” by unknown author is licensed under CC BY-NC 4.0. Access for free at https://ecampusontario.pressbooks.pub/introductiontoipcp/chapter/40/ ↵
- Department of Health. (n.d.). Chain of infection in infection prevention and control (IPAC). The Government of Nunavut. https://www.gov.nu.ca/health/information/infection-prevention-and-control ↵
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- Office of Infectious Disease and HIV/AIDS Policy. (n.d.). Health care-associated infections. U.S. Department of Health & Human Services. https://www.hhs.gov/oidp/topics/health-care-associated-infections/index.html ↵
The process of how an infection spreads based on six links of transmission: Infectious Agent, Reservoir, Portal of Exit, Modes of Transmission, Portals of Entry, and Susceptible Host.
Microorganisms, such as bacteria, viruses, fungi, or parasites that can cause communicable disease.
The host in which infectious agents live, grow, and multiply.
A condition when a person carries an infectious agent but is not symptomatic or ill.
Person who is colonized with an infectious agent but who is not ill.
The route by which an infectious agent escapes or leaves the reservoir.
The way an infectious agent travels to other people and places.
The route by which an infectious agent enters a new host.
A person at elevated risk of developing an infection when exposed to an infectious agent.
An infection that develops in an individual after admission to a health care facility or undergoing a medical procedure.
