When an individual moves into a nursing home, it can be a complicated, stressful, and sometimes confusing time for them and their loved ones. Because nurse aides spend more time with residents than any other staff member, your actions are critical to help ease their worries associated with a change in their environment.
Reflective Activity
Reflect about a time when you moved, changed schools, started a new job, or went to a new place on your own. What things made you feel more comfortable during those transitions? Applying how you felt during those experiences can help you empathize with and provide peace of mind for anyone experiencing a transition.
In addition to experiencing a new environment, newly admitted residents have also typically had a recent major change in cognitive or physical functioning. They are adjusting to not only a new environment but also to how they feel, think, and move. Actions that were previously taken for granted, such as walking, eating, and performing self-care, now require assistance from others. Review the activity in the Chapter 1 subsection “Managing Clients’ and Family Members’ Stress” to increase your awareness of factors that may affect a resident’s outlook and the ways you can improve their quality of life.
As a nurse aide, you can be a major factor in promoting better outcomes for residents by making observations related to their nutritional intake, physical activity, and psychosocial well-being and communicating these observations to the nurse. The Fulmer SPICES tool is a good framework for promoting health in the older adult population. SPICES is an acronym that stands for observing the following aspects that can affect well-being for older adults: Sleep, Problems eating, Incontinence, Confusion, Evidence of falls, and Skin Breakdown[1]:
- Sleep: Older adults need 7-9 hours of sleep per day. To promote good sleep, control environmental factors such as noise, lighting, and temperature. Report sleep disturbances such as excessive snoring or gasping for air or if the resident states they don’t feel rested on awakening.[2]
- Problems Eating: Report issues with chewing and swallowing during meals, as well as residents’ food preferences. Insufficient nutritional intake can lead to skin breakdown issues, infection, and an overall decline in function. More information about eating problems can be found in Chapter 5.
- Incontinence: Incontinence is a lack of voluntary control over urination or defecation. Offer toileting to your residents at least every two hours and on their request. Check incontinence products at least every two hours, especially for those residents with communication problems. More information about incontinence can be found in Chapter 5.
- Confusion: Report any new onset of confusion because it can be a sign of infection. An example of a resident with new confusion would be not knowing the day of the week or where they are when normally they are aware and oriented.
- Evidence of Falls: Report any new weakness or difficulty in transferring from bed to wheelchair or a change in the ability to walk. Read more about fall prevention in the “Emergency Situations” section of this chapter and in Chapter 9.
- Skin Breakdown: Damage to the skin is called skin breakdown. Common preventable causes of skin breakdown are immobility and incontinence. For residents who are unable to independently move, reposition them at least every two hours. For residents with incontinence, provide proper hygiene to keep their skin clean and dry. More information about skin breakdown can be found in Chapter 5.
Transitioning to a New Environment
Transitioning to a nursing home environment involves an abrupt change to an individual’s living environment in terms of privacy, size, and personal belongings. See an image of a typical shared room in a nursing home in Figure 3.5.[3] In addition to this change in environment, residents often cannot follow their typical schedule they had at home, although accommodations should be made to meet their preferences as much as possible.

Nurse aids help residents transition to a new environment. When a new admission is expected, a staff member should be at the entry area to greet the individual and their loved ones. The room should be prepared before arrival, which includes sanitization procedures and making the bed. Read more about how to make a hospital bed in the “Skills Checklist” section of this chapter.
Actions to help residents transition to their new environment include the following:
- Introduce the resident to the staff and identify who is responsible for which resident care needs, such as CNAs, dietary aides, activities personnel, nurses, etc.
- Provide a tour of the facility.
- Show the resident where they can find the daily schedule of events and activities.
- Assist the resident in organizing their belongings and arranging their room to fit their needs and preferences.
- Introduce their roommate if they are sharing a room.
- If possible, arrange to have a resident mentor. A resident mentor is another resident who can answer questions and encourage interaction.
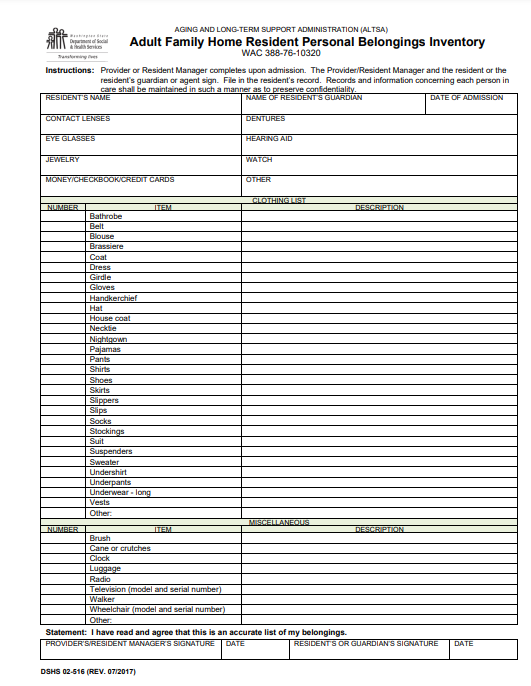
Every facility has their own admission procedures, but a common requirement is the completion of a written inventory of the resident’s belongings. This inventory is typically done by the nurse aide depending upon the care setting. See an example of a Resident Personal Belongings Inventory used in an adult family home in Figure 3.6.[4]
- Aronow, H. U., Borenstein, J., Haus, F., Braunstein, G. D., & Bolton, L. B. (2014). Validating SPICES as a screening tool for frailty risks among hospitalized older adults. Nursing Research and Practice, 2014, 846759. https://doi.org/10.1155/2014/846759 ↵
- Centers for Disease Control and Prevention. (2017, March 2). How much sleep do I need? https://www.cdc.gov/sleep/about_sleep/how_much_sleep.html ↵
- “residentroom.jpg” by unknown for Stratford Manor. Image used under Fair Use. Access for free at https://stratfordrehab.com/ ↵
- “Adult Family Home Resident Personal Belongings Inventory (Residential Care Services)” by Washington State Department of Social and Health Services is in the Public Domain. Access for free at https://www.dshs.wa.gov/office-of-the-secretary/forms ↵
An acronym that stands for observing the following aspects of well-being for older adults: Sleep, Problems eating, Incontinence, Confusion, and Evidence of falls.
A lack of voluntary control over urination or defecation.
Damage to the skin due to common preventable causes like immobility and incontinence.
A resident who can answer questions and encourage interaction for a new resident recently admitted to a long-term care facility.
