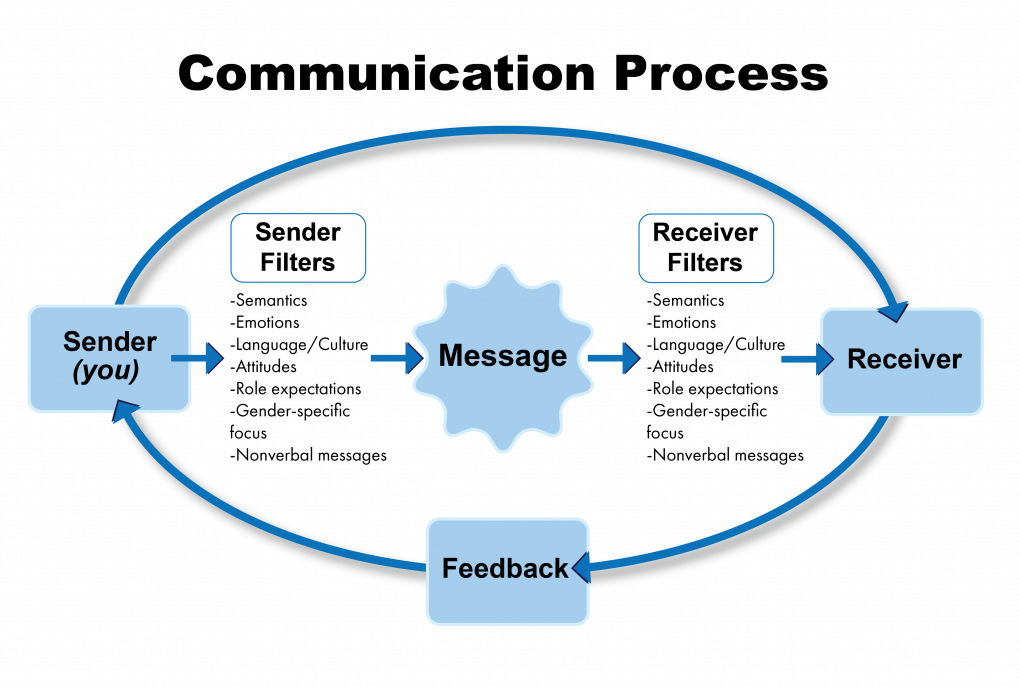
Communication is a process by which information is exchanged between individuals through a common system of symbols, signs, or behavior.[1] In the health care setting, good communication is the foundation to trusting relationships that improve client outcomes. It is the gateway to providing holistic care. Holistic care addresses a client’s physical, emotional, social, and spiritual needs.[2] The communication process involves a sender, the message, and a receiver. See Figure 1.1[3] for an illustration of the communication process.
Verbal Messages
There are many aspects of the communication process that can alter the delivery and interpretation of the message. These aspects relate to the language and experience of both the sender and receiver, referred to as semantics. People typically make reference to things they are familiar with, including landmarks, popular culture, and slang. Barriers can occur even when both parties in the conversation speak the same language. For example, if you asked a person who has never used the Internet to “Google it,” they would have no idea what that means.
Nonverbal Messages
Nonverbal messages, also referred to as body language, greatly impact the conversational process. Nonverbal communication includes body language and facial expressions, tone of voice, and pace of the conversation. See Figure 1.2[4] for an illustration of body language communicating a message. Nonverbal communication can have a tremendous impact on the communication experience and may be much more powerful than the verbal message itself. You may have previously learned that 80% of communication is nonverbal communication. The importance of nonverbal communication during conversation has been broken down further, estimating that 55% of communication is body language, 38% is tone of voice, and 7% is the actual words spoken.[5] If the sender or receiver appears disinterested or distracted, the message or interpretation may become distorted or missed.

Health care professionals assess receivers’ preferred methods of communication and individual characteristics that might influence communication and then adapt communication to meet the receivers’ needs. For example, nursing assistants adapt verbal instructions for adult patients with cognitive disabilities. Although the information provided might be similar to that provided to a patient without disabilities, the way the information is provided is adapted based on the patient’s developmental level. A nursing assistant may ask a cognitively intact person, “What do you want for lunch?” but adapt this information for someone with impaired cognitive function by offering a choice, such as “Do you want a sandwich or soup for lunch?” This adaptation allows the cognitively impaired patient to make a choice without being confused or overwhelmed by too many options.[6] Read more about developmental levels in the “Human Needs and Developmental Stages” section of this chapter.
Communication Styles
In addition to using verbal and nonverbal communication, people communicate with others using one of three styles. A passive communicator puts the rights of others before their own. Passive communicators tend to be apologetic or sound tentative when they speak and often do not speak up if they feel as if they are being wronged. Aggressive communicators, on the other hand, come across as advocating for their own rights despite possibly violating the rights of others when communicating. They tend to communicate in a way that tells others their feelings don’t matter. Assertive communicators respect the rights of others while also standing up for their own ideas and rights when communicating. An assertive person is direct, but not insulting or offensive.[7]
Assertive communication refers to a way of conveying information that describes the facts and the sender’s feelings without disrespecting the receiver’s feelings. Assertive communication is different from aggressive communication because it uses “I” messages, such as “I feel…,” “I understand…,” or “Help me to understand…,” to address issues instead of using “you” messages that can cause the receiver to feel as though they are being verbally attacked. Using assertive communication is an effective way to solve problems with patients, coworkers, and health care team members. For example, instead of using aggressive communication to say to a coworker, “You always leave your patients’ rooms a mess! I dread following you on the next shift,” an assertive communicator would use “I” messages. The assertive communicator might say, “I feel frustrated spending the first part of my shift decluttering patients’ rooms. Help me understand the reasons why you don’t empty the wastebaskets and clean up the rooms by the end of your shift.”[8]
Overcoming Communication Barriers
It is important to reflect on personal factors that influence your ability to communicate with others effectively. There are many factors that can distort the message you are trying to communicate, resulting in your message not being perceived by the receiver in the way you intended. When communicating, it is important to seek feedback that your message is clearly understood.[9] Nursing assistants must be aware of these potential barriers and try to reduce their impact by continually seeking feedback and checking understanding. Review common communication barriers in the following box.
Common Barriers to Communication in Health Care[10]
- Jargon: Avoid using medical terminology, complicated wording, or unfamiliar words. When communicating with patients, explain information in common language that is easy to understand. Consider any generational, geographical, or background information that may change the perception or understanding of your message.
- Lack of attention: It is easy to become task-centered rather than person-centered when caring for multiple residents. When entering a patient’s room, remember to use preprocedural steps and mindfully focus on the person in front of you to give them your full attention. Patients should feel as if they are the center of your attention when you are with them, no matter how many other things you have going on.
- Noise and other distractions: Health care environments can be very noisy with people talking in the room or hallway, the TV blaring, alarms beeping, and pages occurring overhead. Create a calm, quiet environment when communicating with patients by closing doors to the hallway, reducing the volume of the TV, or moving to a quieter area, if possible.
- Light: A room that is too dark or too light can create communication barriers. Ensure the lighting is appropriate according to the patient’s preference.
- Hearing and speech problems: If your patient has hearing or speech problems, implement strategies to enhance communication, including assistive devices such as eyeglasses, hearing aids, and any communication aids such as whiteboards, photobooks, or microphones.
- Language differences: If English is not your patient’s primary language, it is important to seek a medical interpreter and provide written handouts in the patient’s preferred language when possible. Most agencies have access to an interpreter service available by phone if they are not available on-site.
- Differences in cultural beliefs: The norms of social interaction vary greatly in different cultures, as well as the ways that emotions are expressed. For example, the concept of personal space varies among people from different cultural backgrounds. Some people prefer to stand very close to one another when speaking whereas others prefer a distance of a few feet. Additionally, some patients are stoic about pain whereas others are more verbally expressive when in pain.
- Psychological barriers: Psychological states of the sender and the receiver affect how the message is sent, received, and perceived. Consider what the receiver may be experiencing in the health care setting and what may change your delivery of your message. Being rushed, distracted, and overwhelmed are just a few things that can affect your message and its understanding.
- Physiological barriers: It is important to be aware of patients’ potential physiological barriers when communicating. For example, if a patient is in pain, they are less likely to hear and remember what was said. If the patient is receiving pain medication, be aware these medications may alter their comprehension and response.
- Physical barriers for nonverbal communication: Providing information via email or text is often less effective than face-to-face communication. The inability to view the nonverbal communication associated with a message, such as tone of voice, facial expressions, and general body language, often causes misinterpretation of the message by the receiver. When possible, it is best to deliver important information to others using face-to-face communication so that nonverbal communication is included with the message.
- Differences in perceptions and viewpoints: Everyone has their own beliefs and perspectives and wants to feel “heard.” When patients feel their beliefs or perspectives are not valued, they often become disengaged from the conversation or their plan of care. Information should be provided in a nonjudgmental manner, even if the patient’s perspectives, viewpoints, and beliefs are different from your own.
- Merriam-Webster. Communication. https://www.merriam-webster.com/dictionary/communication ↵
- Jasemi, M., Valizadeh, L., Zamanzadeh, V., & Keogh, B. (2017). A concept analysis of holistic care by hybrid model. Indian Journal of Palliative Care, 23(1), 71–80. https://doi.org/10.4103/0973-1075.197960 ↵
- “Communication Process” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Boulder_Worldcup_Vienna_29-05-2010a_semifinals090_Akiyo_Noguchi,_Anna_Stöhr.jpg” by Manfred Werner - Tsui is licensed under CC BY-SA 3.0 ↵
- Thompson, J. (2011). Is nonverbal communication a numbers game? Psychology Today. https://www.psychologytoday.com/us/blog/beyond-words/201109/is-nonverbal-communication-numbers-game ↵
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- This work is a derivative of Human Relations by LibreTexts and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵
- SkillsYouNeed. (n.d.). Barriers to effective communication. https://www.skillsyouneed.com/ips/barriers-communication.html ↵
A process by which information is exchanged between individuals through a common system of symbols, signs, or behavior.
Addresses a patient's physical, emotional, social, and spiritual needs.
Includes body language and facial expressions, tone of voice, and pace of the conversation.
Puts the rights of others before their own.
Come across as advocating for their own rights despite possibly violating the rights of others when communicating.
Respect the rights of others while also standing up for their own ideas and rights when communicating.
A way of conveying information that describes the facts and the sender’s feelings without disrespecting the receiver’s feelings.
